Why Vitamin C is the Most Underrated Nutrient for Heart Health
Vitamin C is everywhere—but when it comes to heart health, it's wildly underrated. We think we understand it. We don’t. And what I found when I dove into the science shocked me.
Vitamin C is everywhere—your orange juice, your multivitamin—but when it comes to heart health, it's wildly underrated. We think we understand it. We don’t. And what I found when I dove into the science shocked me. But we’re going to unravel that mystery together and arm you with practical insights to help your heart.
And — if you can make it through to the end — I have a reward for you. But you do need to watch the full video to fully appreciate and understand the reward.
But first, a quick hat-tip to what had me running down this rabbit hole. I recently wrote a newsletter on Lp(a) (click HERE) that ended up being my most popular to date. I encourage you to check it out if you’re interested in heart health.
Anyway, here’s what you need to know: Lp(a) is like LDL’s evil twin—the one that went to villain school and graduated top of its class in clotting. And, Lp(a) is that’s thought to be genetically cemented. It’s become the “new hotness” in the cardiology world, perhaps because there are five drugs in development to radically lower Lp(a). (Yes, the spotlight of medicine is driven by economics. That’s a fact, not a judgement).
However, some people have success lowering Lp(a) with high-dose vitamin C supplementation. Weird, right?
Well, it makes sense. And that’s where we are going to start our journey into nutrition and biology, after I give you a roadmap of all we’re going to cover, which I’ve broken into 8 chapters:
Vitamin C & Lp(a) – Nature’s substitution
Vitamin C & Heart Disease – What the human data say
Vitamin C & oxLDL – Can it stop cholesterol from turning toxic?
Vitamin C & Nitric Oxide – Why your blood vessels care
Mechanism Summary – Piecing together the puzzle
Vitamin C Dosing – How much do you really need?
Vitamin C & Lysine – Batman & Robin
Puzzling Together the Protocol
Before we dig into this topic, I want to warn you: the deeper you go in this letter the more complex the topic becomes. If you can up and through chapter 7, you’ve earned my intellectual respect.
*Fun fact pitstops: That said, to diffuse the density a bit and keep your attention, I’m trying something new as well: “fun fact pitstops.” Let’s C if you like them!
1. Vitamin C and Lp(a)
Lp(a) is a spherical particle that floats around in the blood. It looks like an LDL particle, except Lp(a) also has a protein tail called apolipoprotein(a). This tail endows Lp(a) with the ability to promote blood clots and is one way in which Lp(a) is thought to promote cardiovascular disease.
But in 1990, the double Nobel Laureate Linus Pauling and his colleague Dr. Rath came up with an interesting idea about Lp(a). They hypothesized that Lp(a) was a surrogate for vitamin C.
*Fun fact pitstops: As a quick terminology lesson, vitamin C is also known as “ascorbate” or ascorbic acid. It got this name given its “antiscorbutic” properties, which means it has the effect of curing scurvy. I mention this so that if you look at the papers I reference, you know that “ascorbate” means vitamin C.
Most mammals can synthesize their own vitamin C. But about 40 million years ago, our primate lineage developed a mutation in the GLO gene that prevents us from synthesizing vitamin C.
Since vitamin C helps to promote wound healing, this would have placed an environmental pressure to develop an alternative means to promote wound healing and halt bleeding. In effect, evolution called for a substitute: Lp(a), which can likewise promote wound healing.
Now, if it were true that Lp(a) is an evolutionary substitute and surrogate for vitamin C, we might expect a pattern whereby animals that can synthesize vitamin C lack Lp(a). This is indeed the case. What’s more, species that have also lost the ability to synthesize vitamin C, including guinea pigs and the European hedgehog, also produce Lp(a).
Across the animal kingdom, there’s a pattern: Where the ability to synthesize vitamin C remains, Lp(a) is missing. Where the ability to synthesize vitamin C is lost, Lp(a) is present.
This provides one comparative evolution argument that Lp(a) is a surrogate for vitamin C.
But the intrigue doesn’t stop there.
Chasing these observations, Pauling and Rath performed experiments where they deprived guinea pigs of vitamin C, which was sufficient to cause them to develop rapid atherosclerosis characterized by plaques filled with Lp(a). Conversely, when guinea pigs were given vitamin C, negligible amounts of Lp(a) could be found in their arteries.
*Fun Fact Pitstop: Linus Pauling championed megadoses of vitamin C, sometimes taking 18,000 mg/day. He lived to 93.
Now I want to shift gears and review some of the human data.
2. Vitamin C and Heart Disease
Epidemiology
One possible implication of the Pauling and Rath hypothesis is that higher levels of vitamin C could slow the progression of heart disease. Exactly how it does so with respect to Lp(a) modification, and other mechanisms, deserves more unpacking. We will get there, I promise. But let’s first ask whether this general observation holds true: Does vitamin C appear to protect against cardiovascular disease?
In four words: the data are mixed, like feelings about pineapple pizza.
However, there are some positive signals. For example, in the Nurse’s Health Study, vitamin C intake from supplements was associated with lower risk of coronary heart disease. And, in the EPIC study, circulating levels of vitamin C were inversely associated with death from cardiovascular disease and ischemic heart disease. This relationship held true even though almost all the participants were within the clinically normal range for vitamin C levels.
Caveat
One cannot draw cause-effect relationships from these epidemiological studies. And other studies have shown negative results. However, the fact that there is any signal is interesting.
When this is the case, and the data seem confused and inconsistent, I like to ask the questions:
Could it be that there are responders (those who benefit) and non-responders (those who do not)?
If so, what determines who is a responder?
These are important questions to answer because sometimes lumping diverse groups of people can lead us to lose sight of biological truth in the haze of biological heterogeneity.
We will return to this idea of responder vs. non-responder momentarily, after we discuss the results of some controlled trials and mechanisms by which vitamin C may be cardioprotective, beyond Lp(a).
*Fun Fact Pitstop: Vitamin C increases non-heme iron absorption (the kind from plants), which is crucial for vegetarians and vegans. Add lemon to your spinach.
Controlled Trials
There have been several successful controlled trials showing benefits of vitamin C supplementation on heart health.
i. For example, in one double-blinded randomized controlled trial on 46 patients with coronary artery disease, one group was given a single dose of 2 grams of vitamin C and longer-term treatment with 500 mg of vitamin C versus a placebo control. The outcome of interest in this study was flow-mediated dilation (FMD), which refers to the widening of an artery in response to an increase in blood flow. This is a non-invasive test used to assess the function of the lining of blood vessels and blood vessel health.
They found both single dose and long-term treatment with vitamin C improved blood vessel function (FMD). The positive effect was also generalized to men and women, and those taking and not taking cholesterol-lowering medications.
ii. As another example, in a randomized trial in patients undergoing a blood filtering procedure called hemodialysis, patients were randomized to receive a placebo or one of two doses of vitamin C—300 mg or 600 mg—given intravenously (directly into the blood) three times per week for 3 months. Because of the nature of these patients, they had all undergone a procedure (angioplasty) that widens their blood vessels. And a major concern after this procedure is that the vessel will clot up again. This is called “restenosis.”
Simplifying and setting aside the jargon: the desired outcome and hypothesis was that vitamin C would slow the rate at which the blood vessels narrow and clog up. Indeed, higher-dose vitamin C significantly slowed restenosis by half, keeping the vessels open wider and for longer.
iii. And in yet another 6-year study that measured atherosclerosis progression by carotid intima-media thickness (CIMT), supplementation with vitamin C and vitamin E slowed progression of atherosclerosis by 26%.
The big-picture point is that, in both epidemiological literature and controlled trial literature, there are signs that vitamin C slows the progression of cardiovascular disease. Now, let’s return to mechanisms.
3. Vitamin C and oxLDL
In addition to potentially reducing —or ‘diffusing’ (more on that below)—Lp(a), vitamin C acts as an antioxidant and can therefore reduce oxidative damage to the blood vessel lining, proteins and fragile fats.
This includes reducing oxidized LDL (oxLDL). In one controlled trial, supplementation with 500 mg per day of vitamin C lowered oxLDL from 87 U/L to 71 U/L, representing an 18% reduction, with no significant change in overall LDL cholesterol levels.
Additionally, vitamin C can act downstream to protect smooth muscle cells in blood vessels from the harmful effects of oxLDL. A key feature of atherosclerotic plaques are necrotic (dead) cores, including the death of smooth muscle cells in the blood vessel wall. One study found that vitamin C defended against the death of smooth muscle cells when exposed to oxLDL, providing another potential protective benefit against atherosclerosis.
4. Vitamin C and NO
Recall earlier we reviewed a trial where vitamin C improved blood vessel function. If you’re curious—and I know you are—then perhaps you were scratching your chin and asking yourself the question, “But how?”
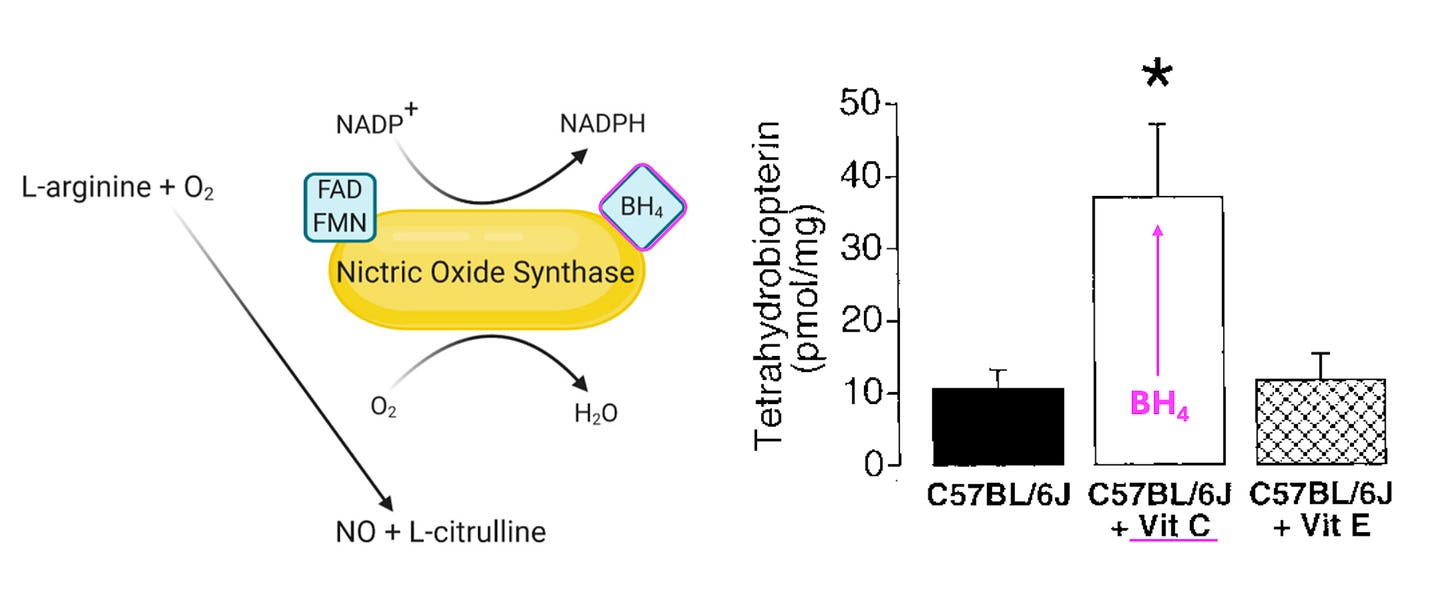
A key signaling molecule in blood vessels is called nitric oxide (NO). It’s a gaseous hormone that helps blood vessels flex and expand, promoting proper blood flow and nutrient delivery. NO is synthesized by nitric oxide synthase (NOS) enzymes. And NOS enzymes require ‘co-factors,’ or molecular assistants. One key NOS co-factor is called tetrahydrobiopterin, or BH4 for short.
Data show that vitamin C can stabilize BH4, thus improving the function of NOS and increasing NO production. This, in turn, can support proper blood vessel function, as reflected in the human trial we reviewed earlier.
The rest of this letter will review:
A Summary of Mechanisms
Optimal Dosing of Vitamin C
Whole Food sources, sorted by Vitamin C density and Vitamin C/Carb Ratio
The Synergy between Vitamin C and Lysine
An Announcement
Keep reading with a 7-day free trial
Subscribe to StayCurious Metabolism to keep reading this post and get 7 days of free access to the full post archives.