Lp(a) Explained: Genetics, Risk, and What You Can Actually Do
My Lp(a) is 165 nmol/l, putting me in the "high risk" category. That's why I needed to know more. Let's discover Lp(a): what it is, why it matters, and what you can do to reduce your risk.
By now, you’ve probably heard the term Lp(a). But to get everyone up to speed, Lp(a) is a major risk factor for heart disease. In particular, it’s a causal risk factor for “atherosclerosis,” the buildup of plaque in the arteries of your heart. On a per particle basis, it’s thought to be 6X as atherogenic as LDL particles.
Now, two more things to know about Lp(a):
Its levels are largely genetically determined
There aren’t many medications or lifestyle treatments to modify Lp(a)
So, what do you do if you’re genetically cursed, like me? With levels of 165 nmol/l, thanks to my dad, I’m in the “severe” risk catagory.
Well, by the end of this letter, I promise on my own heart health, you’ll have a much stronger understanding of Lp(a): what it is, why it matters, and what you can do to reduce your risk of heart disease.
Roadmap
This letter will progress in 8 chapters:
Defining Lp(a)
Guidelines on Measuring Lp(a) & Risk Thresholds
Medications in Development to Lower Lp(a)
How to Reduce Cardiovascular Risk
How Statins Increase Lp(a) and What is Means
Saturated Fat Lowers Lp(a)?
Oxidized Phospholipids: The Cargo of Lp(a)
Nuance Notes for the Nerds
Defining Lp(a)
To understand Lp(a) you first need to understand a better-known lipoprotein particle, the LDL particle. LDL particles are spheres that carry fat and cholesterol around the bloodstream. A core feature of both LDL and Lp(a) is an ApoB lipoprotein that gives the particles function. In fact, the broader class of particles floating in the bloodstream that includes both LDL and Lp(a) is called “ApoB-associated lipoprotein particles.” That makes sense, right?
Now, here’s the critical difference between LDL and Lp(a): Lp(a) has a “tail.”
That tail is an additional protein called apolipoprotein(a) (apo(a) in the graphic below), which is coded in your DNA by the LPA gene. The apolipoprotein(a) “tail” attaches to the ApoB with a bond (called a “disulfide bridge” for the need-to-know nerds).
So, to quickly review:
LDL and Lp(a) are both particles containing ApoB. But Lp(a) has the addition of an apolipoprotein(a) “tail” attached to the ApoB.
What does the apolipoprotein(a) tail on Lp(a) do?
While the functions of apolipoprotein(a) aren’t fully understood, this protein tail does inhibit the breakdown of blood clots, effectively making the blood more “clotty.”
Specifically, lipoprotein(a) particles could, via its tail, attach to blood clots (“thrombus,” in the graphic below) that can block blood vessels and promote their growth, leading to increased risk of cardiovascular disease.
Evolution Kinda’ Screwed Me
Evolutionarily, this “pro-clottiness” could have helped younger individuals survive injury.
*Aside: It’s also worth noting that Lp(a) developed during evolution twice, independently: in old world monkeys and in guinea pigs, an example of convergent evolution wherein two different lineages each developed the same adaptation to improve reproductive fitness.
Sadly, evolution doesn’t optimize for long healthy lives per se. So, the cost of evolving the Lp(a) particle appears to be increased risk of heart disease later in life.
The point: just because something was adaptive “back then” doesn’t mean it’s adaptive today.
Anyway, it’s not helpful to whine about how evolution screwed me. It’s more important for you to understand that, in this case, your genes strongly determine your Lp(a) levels.
Concentrations of lipoprotein(a) are more than 90% genetically determined with minimal influence from lifestyle.
Most of this variation comes from the LPA gene coding for apolipoprotein(a) and something called “Kringle” repeats.
*Aside: If this sounds like a pastry to you, it’s because it is a Danish variety of pretzel. This isn’t a coincidence. The Kringle repeats in the apolipoprotein(a) tail of Lp(a) are named after that pretzel because they have similar structure. Aside over.
Remember: Longer Tail = Lower Levels
In general, there is an inverse association between the number of Kringle repeats, i.e. size of the apolipoprotein(a) tail, and Lp(a) levels.
Simply: Longer Lp(a) tail = Lower Lp(a) levels.
This is because Lp(a) particles with longer tails are more likely to be degraded in the liver before being released into the bloodstream.
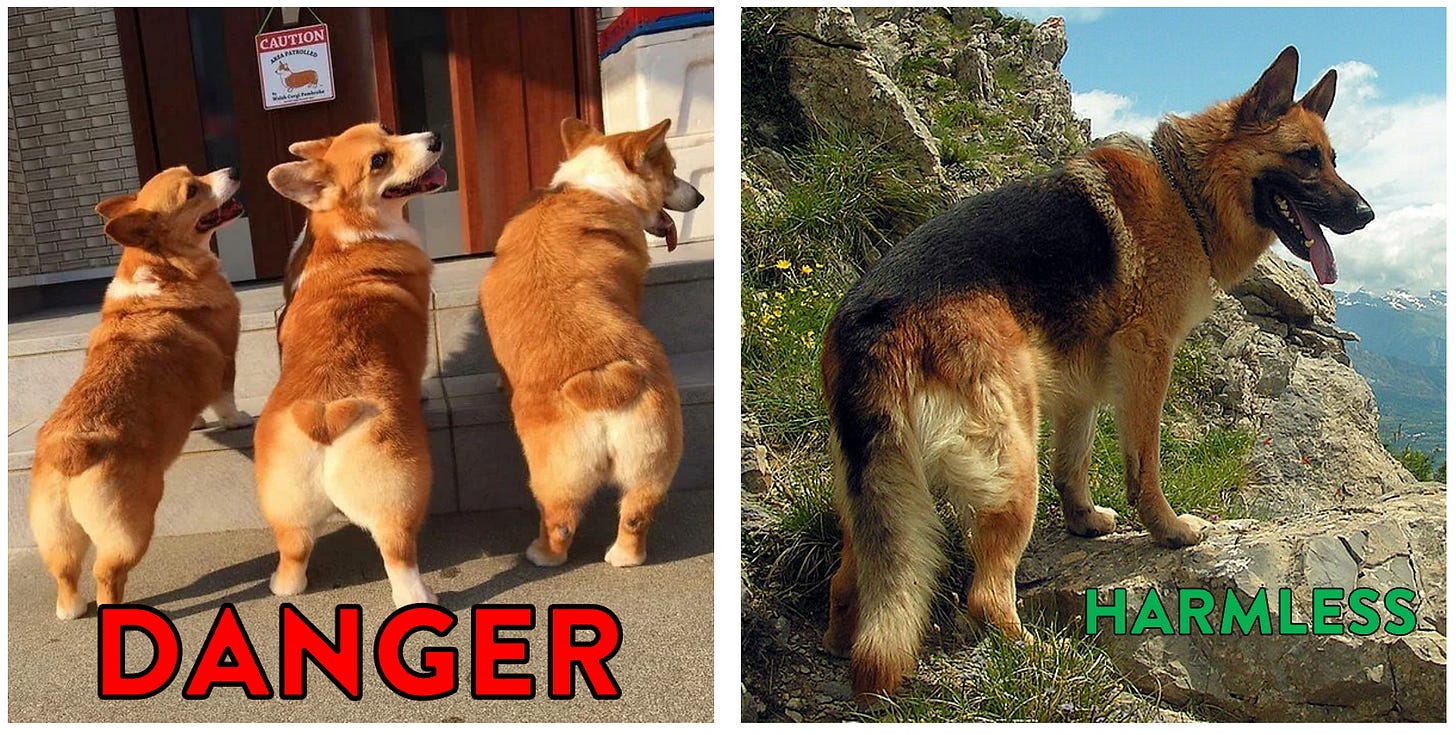
*Analogy (Corgi Butts): Call me goofy, but I imagine it as if you have either a dense pack of Corgis (short tails) floating around in the bloodstream versus one or two German Shepherds (long tails). Except, in this comical case, the Corgis are the dangerous canines.
Guidelines for Measuring Lp(a) and Risk Thresholds
Now that you understand what Lp(a) is, should you measure it? Yes.
Guidelines from the United States, Europe, Canada, China, and India all suggest measuring Lp(a) at least once to include in overall risk assessment.
Now, what are the numbers you should look for on your lab report? How high is too high?
Well, first it is worth noting different reports use different units, either nmol/L or mg/dL. To convert between these, use the formula:
Lp(a) in nmol/L = Lp(a) in mg/dL × 2.18 – 3.83
*Aside: Truth be told, the different units reflect slightly different measures (particle number vs total mass), but this conversion will get you pretty close.
It’s considered that people with Lp(a) levels >30 mg/dL (62 nmol/L) are at slightly increased risk; those with >50 mg/dL (105 nmol/L) are at clinically meaningful increased risk; and those with >90 mg/dL (190 nmol/L) are at severely increased risk.
In reality, the risk associated with high Lp(a) is a continuous spectrum, but we humans like hard cut points.
And, importantly, the risk appears to generalize across races and sexes. So, in theory, the same Lp(a) should confer similar risk in everyone. As we will get into in our later chapters, that’s not actually the case. But first…
Medications in Development
While there are no medications currently prescribed to lower Lp(a), there are several in development. These work by either decreasing the expression of the LPA gene coding for the apolipoprotein(a) tail, or by preventing the tail from attaching to ApoB. Most of these medications are small interfering RNA (siRNA) and administered as injections. There is also one pill taken by mouth, called Muvalaplin, that’s a small molecule inhibitor.
In double-blinded randomized controlled trials conducted in patients with elevated Lp(a), the siRNA injectables lowered Lp(a) by as much as 99%, as shown in the graph below (orange and grey lines). The oral medication, which has the benefit of not being an injection, is slightly weaker but still effective, lowering Lp(a) up to 85.8%.
Importantly, the results thus far are primarily looking at reducing the Lp(a) value on a lab sheet, rather than monitoring for actual clinical benefits, like fewer heart attacks and strokes. So, the biomedical community is still in the process of data collection. However, I’d say the results are promising.
*The rest of this letter will review:
How to reduce your risk
How Statins Increase Lp(a) and what this means
The effect of Saturated fat on Lp(a)
Oxidized Phospholipids (the cargo on Lp(a))
Several nuance notes related to Lp(a) size, menopause and hormone replacement therapy, when Lp(a) changes rapidly, interpreting an LDL-C on a lab report in the light of high Lp(a), and ApoE genotype and Lp(a).
If you’re not yet a premium subscriber, I guarantee you’ll get value by taking the leap!
Keep reading with a 7-day free trial
Subscribe to Nicholas’s Substack to keep reading this post and get 7 days of free access to the full post archives.