Meat the Myths: Top 8 Carnivore Diet Misperceptions
This letter will be "rare," and at the same time "well-done." It will be “provocatively reasonable” and will give you basic truths about what carnivore is, and what it is not.
*On popular demand, I now have a video covering the content also covered in this Newsletter. If you prefer to view (20 min), click below. If you prefer to read, please continue to do so.
The Carnivore Diet is rapidly increasing in popularity, and is sparking debates from dinner tables to social media spaces media spaces to the halls of academia.
Is it a path to better health, or is it dangerously misguided? From fiber myths to vitamin C, in this letter you will meat 8 myth about the diet—and why they may not be as clear-cut as you think.
This letter will be unique – one might call it rare – and at the same time well-done.
It will be “provocatively reasonable” and will give you basic truths about what carnivore is, and what it is not.
Myth 1: “There Isn’t Any Evidence Supporting a Carnivore Diet.”
There actually are several research articles on carnivore diet, including a survey study out of Harvard that included 2,029 participants and found “participants reported high levels of satisfaction and improvements in overall health (95%), well-being (66%-91%), various medical conditions (48%-98%).” There were also two recent case series on a carnivore diet for inflammatory bowel disease and anorexia nervosa.
This is evidence, and the results are rather impressive. I should know, I first authored two of them.
It’s true that randomized controlled trials on a carnivore diet have not been conducted. These will likely need to be completed before conventional medicine can recommend a carnivore diet as a metabolic health intervention for specific disorders, like autoimmune and inflammatory conditions. All this is to say, the research is in an early stage because the carnivore diet “movement” (yes, I’ll call it that) is relatively young.
But that does not detract from the fact that thousands of people are having positive results with a carnivore diet for a broad range of disorders. These are real people with real stories of suffering and recovery. The next step will be to leverage these powerful stories and early data to inspire and fund randomized controlled trials on a carnivore diet.
As a clinical researcher, I can tell you this is easier said than done, particularly given the stigma around a carnivore diet and – even more so – the fact that Big Pharma isn’t going to toss $10 million at a diet trial when it won’t make them, or the medical system, money given the current business model. That’s not a knock at pharmaceuticals or conventional medicine. It’s just reality.
Myth 2: “You’ll Get Scurvy on a Carnivore Diet because Vitamin C Deficiency.”
While it’s true that it’s difficult to meat the RDA daily dose of 75 – 90 mg of vitamin C eating only meat, there is ~25 ug/g of vitamin C in fresh grass-fed beef. So, eating 2 pounds of meat daily would give ~18mg vitamin C. This is still well below the RDA.
The Math: (25ug/g*454g/lb *2lb)/1,000 = 18mg
However, that doesn’t mean one will necessarily develop vitamin C deficiency or the associated medical condition, scurvy. In fact, even back in 1906, the explorer Vilhjalmur Stefansson lived in the Arctic with the Inuit and consumed an almost entirely carnivore diet for months and was surprised to find that he, and the Inuit, were in excellent health overall and were Scurvy-free. In fact, Stefansson did an experiment where he and a colleague ate nothing meat for a year and ended in “good physical condition [with] no subjective or objective evidence of any loss of physical or mental vigor.”
And, to my surprise, when I did a 6-month carnivore diet myself and then tested my intracellular vitamin C levels, they were normal and on the border of being high!
So, what gives?
Well, generally, the rules of nutrition change when you change metabolic states. Here are two mechanisms.
The intake of sugar can reduce the uptake of vitamin C. So, when you’re on a very low carb sugar-free diet, your vitamin C requirements may be reduced.
The antioxidant systems of the body, including endogenous antioxidants (like glutathione) and exogenous antioxidants (like vitamin C), rely on a molecule called NADPH to renew them. Carbohydrate restriction to the point of ketosis can boost levels NADPH, providing a way by which vitamin C could effectively be recycled.
This vitamin C example is just one example of how specific nutrient requirements change depending on metabolic state. So, in my opinion, we should be mindful of this fact and not assume that just because intake of a nutrient doesn’t hit the “recommended value,” that intake might not be perfectly sufficient in a different metabolic state.
Myth 3: “You Need Fiber or You Won’t Poop.”
This is an easy myth to debunk. Just live with someone who is carnivore and ask to inspect their toilet bowl. A large part of the mass of your stool is actually dead bacteria. And, while a majority of the nutrition one consumes on a carnivore diet should be absorbed in the small intestine and overall fecal mass will decrease, you’ll still poop.
On a related topic, studies suggest that fiber elimination can help manage the symptoms of irritable bowel syndrome (IBS) with constipation. Reading from the linked paper, “Idiopathic constipation and its associated symptoms can be effectively reduced by stopping or even lowering the intake of dietary fiber.”
And fiber elimination can even help put inflammatory bowel disease (IBD) into remission. So, in some cases, there can be a therapeutic aspect.
That said – and I want to be clear about this – this does not mean that fiber is bad or that a long-term zero fiber diet couldn’t have negative consequences on the microbiome. The high-level way I think about it is as follows: ecosystems – be it a rainforest, coral reef, or your microbiome – are generally most resilient and healthy when they’re diverse. And giving more food and fodder to your microbiome, in the form of pre- and probiotics, fermentable fibers, polyphenols, etc. can help support that diversity. So, all things being equal, I’d gamble on chronic fiber elimination being a risk.
That said, I don’t eat much fiber. Why?
Well, because of something I alluded to earlier.
Given my personal history with IBD and IBS, and the symptoms I’ve suffered through, I feel much better on a low-fiber diet. That’s my choice given my circumstance and given my current goals. And there are many like me who feel better on low or no fiber diets.
So, I come back to “all else being equal.” But they almost never are. And in terms of the long-term consequences of zero fiber diets. Well, we simply don’t know. But if the carnivore diet remains as poopular as it is today, we will surely find out.
Myth 4: “A Carnivore Diet Will Harm Your Athletic Performance.”
This one is a bit funny because I can think of a few human carnivores who are absolute athletic beasts.
But speaking to the data, as your body adapts to carbohydrate restriction, your capacity to burn fat increases, reducing demands on muscle glycogen, stores of which in the post-exercise and pre-exercise states will increase on a low-carb diet as the body adapts.
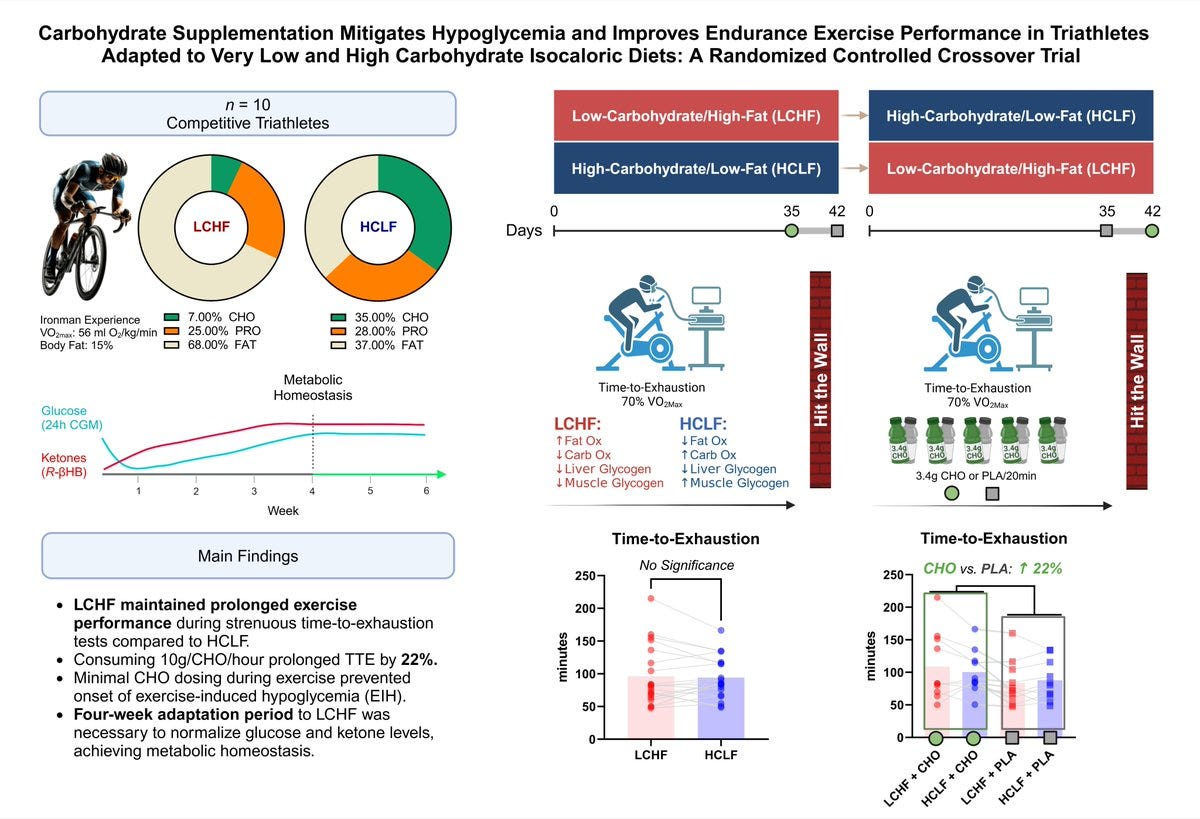
Furthermore, a new study on ironman athletes has debunked the idea that the body needs a high intake of carbohydrates during intense exercise to maintain peak performance.
Now, admittedly in this study, very low dose carbohydrate was supplied but only to offset exercise-induced hypoglycemia. The short of it is that ‘fatigue’ and reduced athletic performance isn’t driven so much by muscle glycogen depletion as it is, likely, from a central nervous system mechanism that can be ‘hacked’ by just giving a tiny bit of carbs during very high intensity exercise to keep the blood supply from dropping… the carb equivalent of ~1/2 tsp of honey per 20 min of intense exercise.
It’s also likely that the dose needed could be even lower (or even zero) in long-time (months) keto-adapted athletes since ketones can offset the need to maintain a higher blood glucose, and longer keto adaptation periods make the body better at ration carb fuel, supplied in small exogenous doses or generated by the body itself.
Myth 5: “A Carnivore Diet Will Give You a Heart Attack.”
Now this myth is a whole kettle of fish unto itself. So, I’ll be brief and link more content (HERE). It’s true, a diet rich in red meat and saturated fat can increase levels of LDL-cholesterol (LDL-C) and the associated marker ApoB, which are independent risk factors for heart disease. I’m not denying that.
However, the extent to which a carnivore diet increases LDL-C and ApoB, or does not, is highly individual.
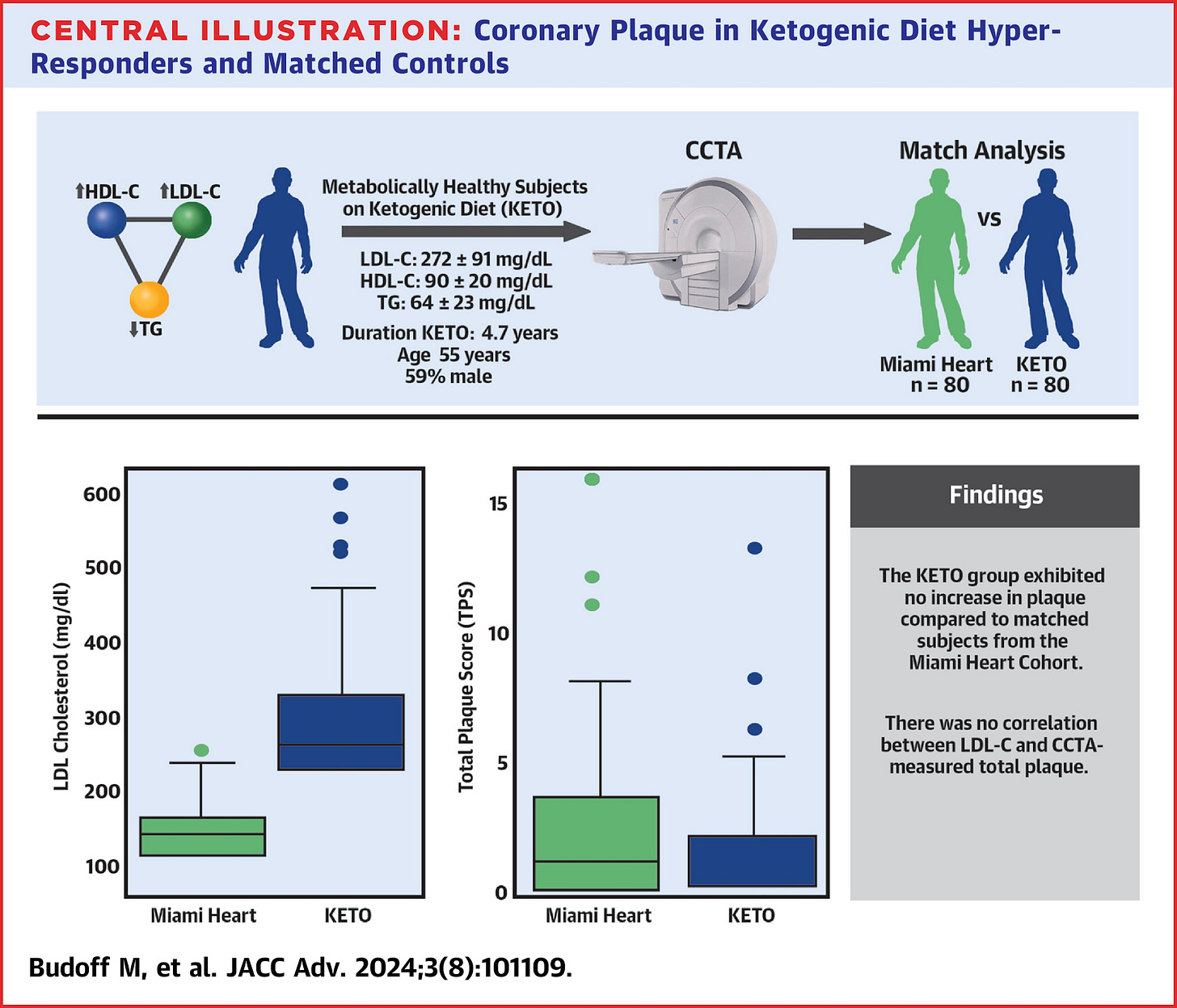
In fact, on these markers alone, some people even see LDL-C and ApoB decrease, especially if they start from a place of obesity and insulin resistance. And for those - generally lean, insulin sensitive people – who do see an increase in LDL-C and ApoB when they go keto or carnivore, we are actively studying their risk in a prospective study using coronary CT angiography to see how rapidly plaque develops.
The early data suggest the risk might not be as great as many would have you believe. That said, these early data don’t dismiss risk entirely. However, neither can one claim – with evidence on this population – that’s it’s a very high-risk population. Again, for more nuances, see these resources. And keep your eyes peeled for our upcoming publications.
And it bears reinforcing, there are many risk factors for heart disease - visceral fat, insulin resistance, inflammation, triglycerides and HDL-C - that can be improved on very low carbohydrate diets, including carnivore.
But the bottom line in different people respond differently. So, it’s worth tracking your biomarkers and considering your individual case, rather than making assumptions. I’m not saying dismiss risk, I’m saying get informed about your personal risk.
Myth 6: “A Carnivore Diet is an Eating Disorder.”
This is easy to debunk. Eating disorders are defined as restrictive eating patterns that impair physical or mental health.
So, if a person cures or goes into remission from a debilitating chronic disease, be it obesity, diabetes, depression, schizophrenia, inflammatory bowel disease using a carnivore diet, then the diet clearly had a positive impact on physical or mental health and is not an eating disorder but an adaptive eating pattern, provided it’s formulated in a sustainable way. And a carnivore diet can be sustainable.
Simply, not eating “normally” is not an eating disorder. In fact, given what “normal” is nowadays, I’d say some “normal” eating patterns could themselves reflect an eating disorder.
And to put the cherry on top of this debunk sundae, we published a case report on the use of a carnivore diet in three remarkable cases of anorexia nervosa. I’ll place a trigger warning on this given some graphic images in the paper. But you should give it a read.
Myth 7: “A Carnivore Diet is Bad for the Brain.”
This myth really started doing the rounds earlier last week as I write this, following on a paper published in Neurology, and a waterfall of media headlines that followed claiming “Red Meat Intake is Linked to Dementia.”
I’ll quickly debunk this ‘major’ study to give you a flavor of how misleading these sorts of reports can be.
The study in question used food frequency questionnaires that lumped foods like lasagna and cheeseburgers in with steak and lamb.
More importantly, there was tremendous healthy user bias: Quoting, “…participants who consumed more red meat had a higher prevalence of current smoking, hypertension, and diabetes and lower levels of dietary quality, education level, [socioeconomic status], physical activity…”
Unprocessed red meat was not linked to dementia or cognitive decline, just processed red meat. But this was somewhat overlooked in the study itself when they attempted to discuss their biological explanation for how red meat could harm the brain, mostly citing topics like saturated fat and TMAO that aren’t specific to processed red meat.
And, if you really want to put sugar in the wound, if you delve into their own citations for statements like, “diets rich in saturated fats can reduce brain-derived neurotrophic factor…” you’ll find the referenced studies literally specify “high-fat sucrose diet.”
So, “TLDR” — A milkshake is not a steak.
Myth 8: “A Carnivore Diet Means…”
One of the reasons a carnivore diet, or red meat intake in general, gets so much flack is because this pattern of eating is conflated with other distinct topics or beliefs. So let me be clear on what a Carnivore Diet does not mean. Eating a carnivore diet for therapeutic purposes Does NOT Mean:
…It’s best for all humans
…It’s good for the microbiome long-term for most people
…Fiber or fruit is “bad” or that carbohydrates are, as a entire macronutrient group, harmful
…Greenhouse gases are pixie dust
…Animal welfare doesn’t matter
…Someone else can’t succeed on a vegan diet.
A carnivore diet is a potent metabolic intervention with particular use cases that deserve further exploration. It is due further rigorous scientific investigation, and the patients who are using it to treat debilitating illnesses do deserve good health, even if their meat-heavy diets counter the dogma and status quo on what’s healthy.
So, stop beefing with the Carnivore Diet—it’s helping people heal.
In closing, I’m not ‘for’ or ‘against’ the carnivore diet, per se. Context and nuance are essential. However, I do feel it’s misunderstood, and that red meat and animal-based foods often get (unfairly) scapegoated and thrown under the (Big Food) Bus.
The Carnivore Diet is not a one-size-fits-all solution, but it challenges conventional nutrition wisdom in powerful ways. Whether you’re curious or critical, I hope this letter offered a clearer view of its myths and potential.
For more insights, check out my new playlist on animal-based diets. Click HERE.
Let’s meat in the middle and recognize the Carnivore Diet deserves more study.











Great article, keep up the good work!
Awesome. I have been keto for 8 years 🙏🏾