Carbs and Codons: Understand Your Genes to Defeat Obesity
We review Mendelian randomization that supports the Carbohydrate Insulin Model of Obesity. Knowledge is Power!
Is obesity a genetic disease? “No,” but also, “Yes.”
I say, “No,” insofar as most cases of obesity are not caused by a single genetic mutation. However, the answer is “Yes” insofar as obesity is a complex disease where different individuals have different genetic susceptibilities that are unveiled through lifestyle.
In fact, any two unrelated people vary from each other at about 4 million sites within our genomes!
So, yes, there’s enormous genetic diversity, and this does impact our predisposition to diseases, obesity included. In this letter, we will not only provide evidence of this fact, but also explain how this knowledge can be used to more precisely and effectively treat obesity in our modern world.
Mendelian Randomization to Test the Carbohydrate Insulin Model (CIM)
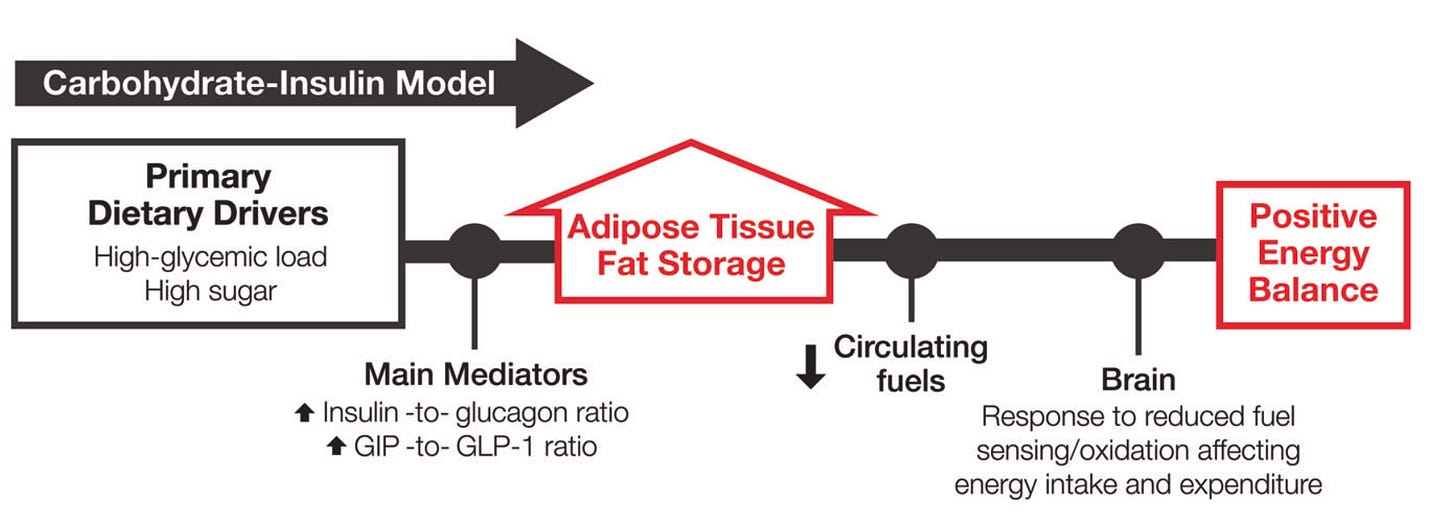
What researchers did in this study was test a key prediction of the Carbohydrate Insulin Model (CIM) using Mendelian randomization.
Let’s unpack each of those terms, staring with the CIM.
The CIM is a mechanistic model of obesity that works as follows: a high glycemic load diet (meaning one that tends to spike blood sugar and blood insulin levels more) gives a hormonal signal to the body (high insulin) to store energy as fat tissue.
In other words, energy (calories) come in, and they’re “triaged:” preferentially towards fat, rather than energy expenditure or lean tissue.
As a downstream consequence, energy expenditure goes down and hunger increases. Thus, while “calories in – calories out = weight change” and thermodynamics is maintained, the calorie imbalance is the result of a primary hormonal disturbance.
In very simple terms, calories count but they do not cause fat gain and obesity. Rather, a “calorie surplus” is the result of the hormone insulin signaling to fat cells to get fat.
This model is supported by multiple lines of evidence, including everything from pre-clinical mechanistic studies to human randomized controlled trials. However, an obvious question remains: why do some people report ballooning up when they eat any carbs, and others seem to eat pasta, bagels, and cookies to their heart's content without gaining excess body fat?
It’s a legitimate question, and one researcher sought to address in this genetics—Mendelian randomization—study.
But what is Mendelian randomization?
Mendelian randomization is a method scientists use to study whether a certain factor (like insulin secretion) causes a particular outcome (in this case, obesity).
It relies on genetic variations (remember those 4 million variable genetics sites from above?) that are assigned randomly by nature’s genetic coin toss to uncover cause-and-effect relationships.
Study Question: So, in this study, the researchers asked the question, “does carbohydrate-stimulated insulin secretion (the amount of insulin released in response to a carbohydrate load) predict obesity?”
If it does, it provides more evidence for the CIM.
Diving into the Methods
In this study, they used MAGIC!
No, actually, they relied on data from the Meta-Analysis of Glucose- and Insulin-related traits Consortium (MAGIC), a previously published meta-analyses on insulin secretion including 26,037 people. They also used data from the United Kingdom Biobank (n =138,541), and a validation cohort, the Cardiology and Metabolic Patient Cohort study at Massachusetts General Hospital (n =1,675).
Using prior knowledge about variations in the human genome, they created genetic risk scores for the traits: (i) carbohydrate-stimulated insulin secretion (how much insulin a person secretes in response to carbs), and (ii) body mass index (BMI).
*Nuance note: the researchers did their due diligence to validate their genetic risk scores in a separate population, basically confirming that the GRS for insulin secretion after a carbohydrate challenge (75 grams of glucose) did indeed predict the amount of insulin that was released and circulating in the blood at 30 minutes.
Mendelian Randomization Results
The researchers found a higher insulin release genetic risk scores did predict higher BMI.
In fact, they even tested slightly different insulin release genetic risk scores in different populations and consistently found - “Yes!” - more insulin release in response to carbs, as influenced by genetics, did predict a higher BMI.
*The above is simplified from Figure 3 in the paper, with labels adjusted ease in interpretation for a general audience. The Insulin-30 Genetic Risk Score refers to “insulin-30-stringent” in the paper, which includes 3 genetic variants.
This is consistent with the CIM: where higher insulin release tells fat cells to store fat, leading to obesity. This puts calories in the passenger seat where a calorie imbalance results, not from “just eating too many calories,” but from the hormonally stimulated growth of fat cells.
Keeping it as simple as possible: Carbs spike insulin → insulin tells fat cells to grow → this leads downstream to increased hunger and decreased energy output.
So, there you have it! Case closed. But not really…
Bi-directional Mendelian Randomization Supports the CIM
The researchers took another very important step.
A limitation of Mendelian randomization is it can confuse causal direction. In other words, to really be certain these results support the CIM in the strongest sense, you’d want to show insulin secretion in response to carbs predicts BMI, but also that the converse isn’t true, i.e. that genetically influenced BMI isn’t predicting insulin secretion in response to carbs.
This is called a bidirectional Mendelian randomization, because you’re asking about the relationship in both directions: genetically influenced insulin secretion → higher BMI, and genetically influenced higher BMI → insulin secretion.
Long story short, they found no statistically significant evidence for the latter, thus supporting the CIM.
“So What” - Codons Over Carbs
This study has a clear practical takeaway: people who secrete more insulin in response to carbs as a result of “unlucky” genetics, will benefit more from carbohydrate restriction in terms of weight loss than those who, because of their “lucky” genetics, secrete less insulin.
In effect, the genetically determine insulin secretion in response to carbs acts as a damage multiplier for that bowl of pasta or donut as far as weight gain goes.
In fact, this conclusion is supported by other studies, including a major human randomized controlled trial called DIETFITS, where those who tended to secrete more insulin were found to benefit more from a reduction in the glycemic loads of their diets.
So, if your DNA dictates you secrete a lot of insulin in response to carbs, it’s worth being mindful of the fact that carbs will hit you harder in terms of weight gain.
I apologize on behalf of biology; Mother Nature’s game isn’t always fair.
But the good news is awareness and knowledge are power!
And having this knowledge enables a precision nutrition approach, and motivation for those who would benefit to swap the breakfast oatmeal and bananas for smoked salmon and avocado, or dinner of Shepard’s pie for a nice filet and roasted vegetables.
I think these data are optimistic, not fatalistic. What about you?
Study Limitations
In closing, I want to mention limitations of this study, as all studies have their caveats.
First, the populations studied were predominantly of European ancestry. Diversifying the population pools will help with the generalizability of these findings, especially to underrepresented minority populations that may be as especially high risk for obesity, possibly owing to group dynamics in insulin secretion and also socioeconomic factors.
Second, these data do not argue that obesity is completely explained by genetically determined insulin secretion interacting with dietary carbohydrates. In fact, in absolute amounts, insulin secretion only predicted a modest proportion of variation in BMI. This is to be expected in a complex trait like obesity. But it is nevertheless worth highlighting.
Third, the human genome isn’t completely annotated and understood. So, we are necessarily missing pieces of the genetic puzzle. Repeating this analysis in 5 or 10 years may reveal even stronger relationships and reveal more actionable genes and insights.
Conclusion
Understanding the intricate interplay between genetics, insulin, and diet is a game-changer in the fight against obesity. This study not only provides compelling evidence for the Carbohydrate Insulin Model but also highlights the potential for precision nutrition to revolutionize how we approach weight management.
While our genetic makeup may predispose us to certain challenges, it also offers a roadmap for personalized interventions. With knowledge in hand, we have the power to make informed dietary choices, turning what might feel like a biological disadvantage into an opportunity for targeted, effective action. Let’s use this insight to take control of our health and redefine what’s possible. #StayCurious #StayCompassionate.
More on this topic
Yesterday, I released a video reviewing data on the “anti-obesity” class of medications, GLP-1 receptor agonists. These aren’t just weight loss drugs. They also have direct anti-inflammatory properties, and in the video I discuss lessons we can learn about metabolism from these medications that goes well beyond “people just eat less.”
And if you’re still not convinced calories don’t cause obesity, I encourage you to check out the below two videos.







knowledge and awareness are power! again and again!
if you know or measure it, you ca change it
thank you for make simple and clear a so complex and delicate topic
Nice article.
Perhaps before potentially labeling a higher insulin response to carbs a “not so good” thing for weight, we should also discuss why a higher insulin response to carbs would have been beneficial for our ancestors.
Genes provide advantages and disadvantages dependent upon the environment they are living in. Perhaps in past generations this higher insulin response enabled people to store more fat for the winter or for famines when carbs or food was scarce.
And now in a different food environment these same genes may harm us if we eat too many carbs year round as opposed to seasonal.
So when it comes to genetics, I like to figure out first why a gene may have helped our ancestors survive and procreate, before trying to figure out why it is now a “not so nice gene” to have.
It’s a different but needed perspective.
Also it would be cool to see how these genes you discussed differ among people whose ancestors lived in different parts of the world, say the difference between living in cooler vs warmer climates, inland vs near oceans.
With genes I don’t see good or bad, I just see different and ask why.